Mental Health Transformation
Together we will improve mental health and wellbeing through thriving, connected communities. Right care, right place, right time.
Over the last few months LPFT and partners from across Lincolnshire have been working together to develop and shape how Mental Health services will look and be delivered in the future. By listening and working with our local communities to understand more about what people want and need; we have been able to bring together a vision for Lincolnshire.
The video below gives an overview of what work has happened so far.
Click on the links below to find out more.
Our vision
To create opportunities for people to thrive; discover & shape their communities; encourage relationships and build a sense of belonging to support their wellbeing.
In the video below Victoria Sleight, Transformation Programme Manager, talks more about the programme and what is already happening across Lincolnshire.
This film is a short visual walk through of the NHS Long-Term Plan commitment on community mental health transformation. The video outlines essential information and learnings on the development of new integrated models of primary and community mental health for people with severe mental illness (SMI). It describes the principles of the already-published Community Mental Health Framework for Adults and Older Adults as per the vision of the Long Term Plan. It also explains the roles of the different organisations that need to work together to develop these models, and the central focus on the needs and involvement of patients, those that care for them, and other experts by experience.
Aims/Objectives/Goals
- Expansion of Integrated Place Based Teams
- Relisation of population health led, clinical delivery model
- Multi-agency and cross sector collaboration to realise collective impact at local level
- Investment in community assets, through co-production with local people
- to develop local support networks
- Up-skilling, training and coaching of local people and clinicians to improve quality of care for people living with SMI
- Co-production of a volunteer & peer support network including people with lived experience
- Continued development of the ‘digital first’ offer
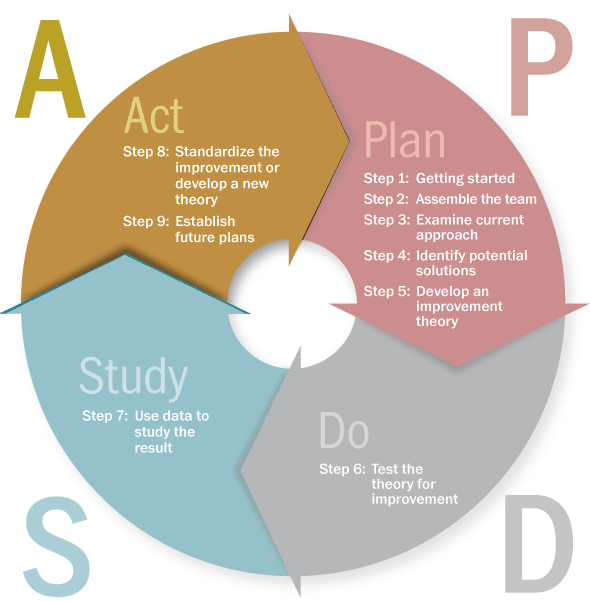
How will we get there
Through the utilisation of continual learning - Plan, Do, Act, Study approach.
Integrated Place Based Teams
An Integrated Place Based Team is a team that sits at the heart of the community and is made up of multiple professionals all working together to support individuals to live the best quality of life possible. They work together to promote self efficiency through a person centred approach and also to bridge the gap between voluntary, health and social care.
Achievements to date
We have:
- Strengthened Partnerships across the Primary, Secondary and Voluntary Sectors
- Embedded a large cultural change package of support across the workforce
- Begun to work with the Recovery College to develop training for the community and the VCSE sector for MH and Wellbeing
- Developed an overarching clinical model of practice that promotes self- efficacy and is a BioPsychoSocial Model that puts the person at the centre
- Started a large scale recruitment plan
- Developed a strong Digital First Offer
- Begun to test new ways of working within our Integrated Place Based Teams
- Embedded new and innovative roles such as Social Prescribing Link Workers, Peer Support Workers and Community Connectors
- Co-located some of our teams to improve conversation and minimise risk and further develop Community Hubs to support accessibility and a strength based approach
- Recognised and invested into the need for localised investment into our VCSE
- Developed a 24/7 MH Matters Helpline that runs 365 days per year
- Established Night light Cafes in some parts of the county
How you can support us
"Be involved, Be open-minded, Be an active listener."
Useful Links
Mental health and primary care networks: understanding the opportunities